Learning Objectives
Upon completion of this chapter, you will be able to:
1. Outline the underlying physiological events that occur with upper respiratory disorders.
2. Discuss the use of drugs that act on the upper respiratory tract across the lifespan.
3. Describe the therapeutic actions, indications, pharmacokinetics, contraindications, most common adverse effects, and important drug–drug interactions associated with drugs acting on the upper respiratory tract.
4. Compare and contrast the prototype drugs with other agents in their class and with other classes of drugs that act on the upper respiratory tract.
5. Outline the nursing considerations, including important teaching points, for patients receiving drugs acting on the upper respiratory tract.

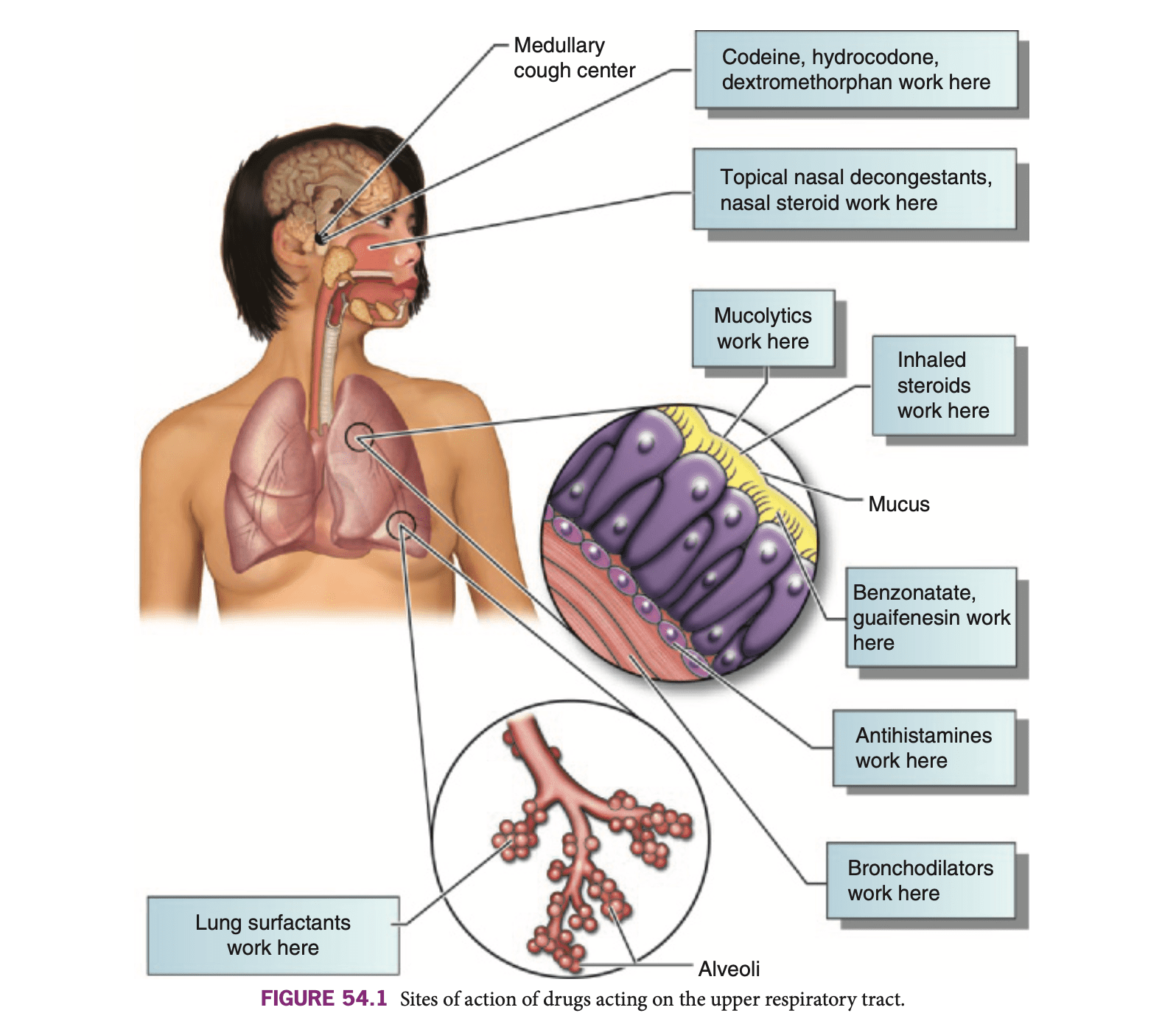
Figure 54.1

Figure 54.2
The drugs that are described in this chapter affect the respiratory system to treat symptoms of allergic or nonallergic rhinitis as well as cough and other symptoms from the common cold, influenza, and other respiratory disorders. They are designed for symptom relief and to keep the respiratory airways patent. They are not designed to treat or cure infection. Figure 54.1 displays the sites of action of these drugs. Figure 54.2 shows the structures of the upper respiratory tract.
Antitussives are drugs that suppress the cough reflex (Table 54.1). Many disorders of the respiratory tract, including the common cold, sinusitis, pharyngitis, and pneumonia, are accompanied by an uncomfortable, unproductive cough. Persistent coughing can be exhausting and can cause muscle strain and further irritation of the respiratory tract. A cough that occurs without the presence of any active disease process or persists aft er treatment may be a symptom of another disease process and should be investigated before any medication is given to alleviate it. Box 54.1 discusses the use of antitussives and other drugs acting on the upper respiratory tract in various age groups.
The traditional antitussives include codeine (generic), hydrocodone (generic), and dextromethorphan (generic), which act directly on the medullary cough center of the brain to depress the cough reflex. Because they are centrally acting, they are not the drugs of choice for anyone who has a head injury or who could be impaired by central nervous system (CNS) depression. Codeine and hydrocodone are opioid agonists that are primarily indicated for pain relief (see Chapter 26). They are used as cough suppressant medications in several combination formulations (Tuxarin ER, Hycodan, and others). They are controlled substances, designated schedule II when used alone and schedule V when used in combination and low amounts.
Other antitussives have a direct effect on the respiratory tract. Benzonatate (Tessalon) acts as a local anesthetic on the respiratory passages, lungs, and pleurae, blocking the effectiveness of the stretch receptors that stimulate a cough reflex.

Codeine, hydrocodone, and dextromethorphan are rapidly absorbed, metabolized in the liver, and excreted in the urine. They cross the placenta and enter human milk. Benzonatate is metabolized in the liver and excreted in the urine. These drugs should not be used during pregnancy and lactation (see “Contraindications and Cautions”).
Antitussives are contraindicated in patients who need to cough to maintain the airways (e.g., postoperative patients and those who have undergone abdominal or thoracic surgery) to avoid respiratory distress. Careful use is recommended for patients with asthma and emphysema because cough suppression in these patients could lead to an accumulation of secretions and a loss of respiratory reserve. Caution should also be used in patients who are hypersensitive to or have a history of addiction to narcotics (codeine, hydrocodone). Codeine and hydrocodone are narcotics and have addiction potential. Patients who need to drive or be alert should use codeine, hydrocodone, and dextromethorphan with extreme caution because these drugs can cause sedation and drowsiness. These drugs should not be used during pregnancy and lactation because of the potential for adverse effects on the fetus or baby, including sedation and CNS depression.
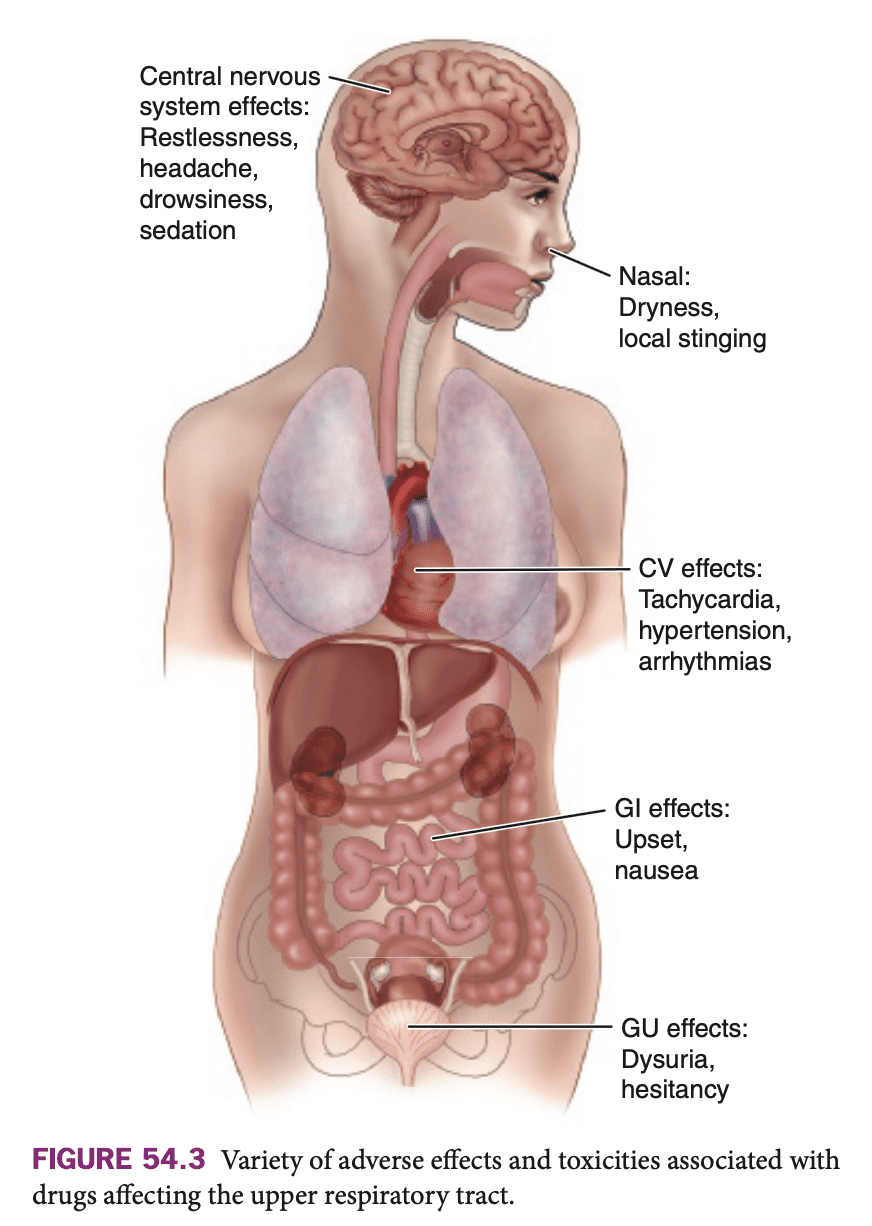
Traditional antitussives have a drying effect on the mucous membranes and can increase the viscosity of respiratory tract secretions. Because they affect centers in the brain, these antitussives are associated with CNS adverse effects, including respiratory depression, drowsiness, and sedation. Other common side effects are nausea, vomiting, and constipation (Fig. 54.3). There is risk of addiction and dependence with the opioid substances. Locally acting antitussives are associated with gastrointestinal (GI) upset, headache, feelings of congestion, and sometimes dizziness. However, when taken at recommended doses, the adverse effects are generally mild.
Dextromethorphan should not be used with monoamine oxidase (MAO) inhibitors; hypotension, fever, nausea, myoclonic jerks, and coma could occur. Concurrent use of the opioid medications with other medications or substances (like alcohol) can increase the risk of respiratory depression, sedation, coma, and even death.

Box 54.1 Focus on Drug Therapy Across the Lifespan
UPPER RESPIRATORY TRACT AGENTS
Children
These drugs are used frequently with children. Most of these agents have established pediatric guidelines. Care must be taken when these drugs are used with children because the risk of adverse effects, including sedation, confusion, and dizziness, is common with children. Cough and cold medications should not be used in children under 4 years of age and should be used with extreme caution in children 4 to 6 years of age.
Because many of these agents are available in OTC cold, flu, and allergy remedies, it is important to educate parents about reading labels and following dosing guidelines to avoid potentially serious accidental overdose. Parents should always be asked specifically whether they are giving the child an OTC or herbal remedy.
Parents should also be encouraged to implement nondrug measures to help the child cope with the upper respiratory problem—drinking plenty of fluids, using a humidifier, avoiding smoke-filled areas and contact with known allergens or irritants, and washing hands frequently during cold and fl u season.
Adults
Adults may inadvertently overdose on these agents when taking multiple OTC preparations to help them get through a cold or flu. They need to be questioned specifically about the use of OTC or herbal remedies before any of these drugs are advised or administered. Adults can also be encouraged to use nondrug measures to help them cope with the signs and symptoms.
The safety for the use of many of these drugs during pregnancy and lactation has not been established. There is a potential for adverse effects on the fetus related to blood flow changes and direct drug effects when the drugs cross the placenta. The drugs may enter human milk and may also alter fluid balance and milk production. It is advised that caution be used if one of these drugs is prescribed when the patient is breast or chestfeeding.
Older Adults
Older adults are frequently prescribed one of these drugs. It is common for older adults to develop adverse effects associated with the use of these drugs, including sedation, confusion, and dizziness. Safety measures may be needed if these effects interfere with the patient’s mobility and balance.
Older adults also are more likely to have renal and/or hepatic impairment related to underlying medical conditions, which could interfere with the metabolism and excretion of these drugs. The dose for older adults may need to be started at a lower level if there is renal and/or hepatic impairment. The patient should be monitored closely, and dose adjustment should be based on the patient’s response.
These patients also need to be alerted to the potential for medication interactions when using OTC preparations and should be advised to check with their health care provider before beginning any OTC drug regimen.

Question
What precautions should be taken when using cough and cold medications in children?
Answer the question above the continue reading. iTELL evaluation is based on AI and may not always be accurate.
Nursing conclusions related to drug therapy might include
● Antitussive drugs suppress the cough reflex by acting centrally to suppress the respiratory cough center or locally as an anesthetic or to increase secretion and buffer irritation.
● Antitussive drugs can cause CNS depression, including drowsiness and sedation.
● Antitussive drugs should be used with caution in any situation in which coughing could be important for clearing the airways.
Decongestants decrease the overproduction of secretions by causing local vasoconstriction to the upper respiratory tract (Table 54.2). Th is vasoconstriction leads to a shrinking of swollen mucous membranes and tends to open clogged nasal passages, providing relief from the discomfort of a blocked nose and promoting drainage of secretions and improved airflow. An adverse effect that accompanies frequent or prolonged use of these drugs is a rebound congestion, technically called rhinitis medicamentosa. The reflex reaction to vasoconstriction is a rebound vasodilation, which oft en leads to prolonged overuse of decongestants.
Decongestants are usually adrenergics or sympathomimetics (see Chapter 30). Topical steroids are also used as decongestants, though they take several weeks to become effective and are more oft en used in cases of chronic rhinitis.
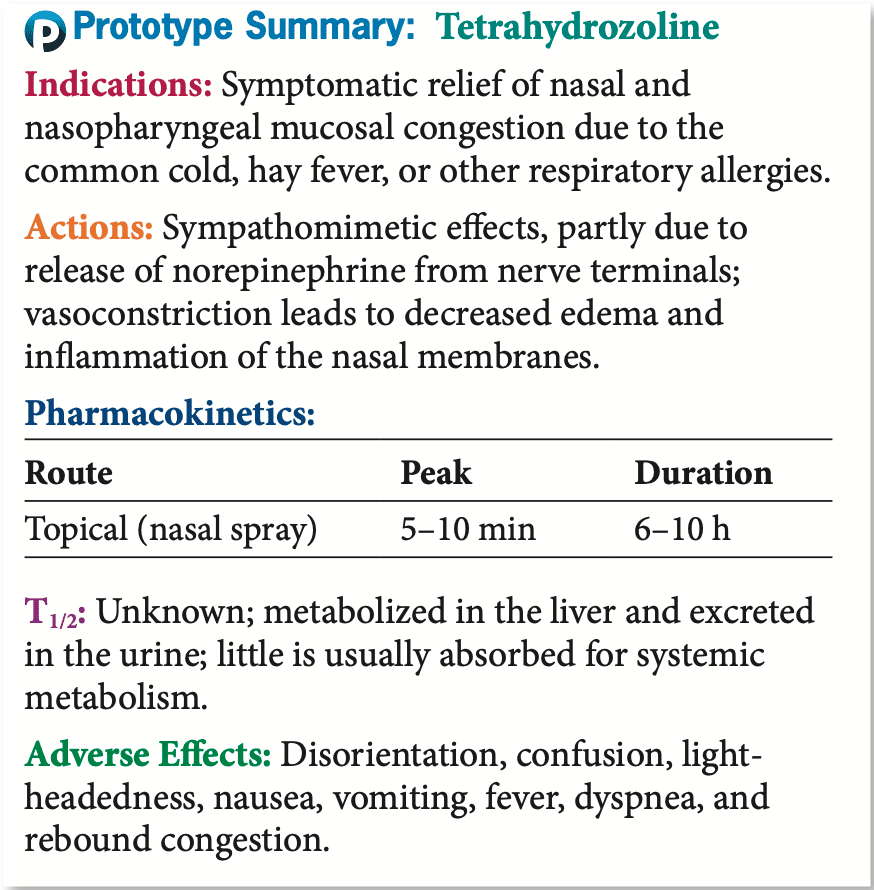
Topical nasal decongestants include naphazoline (Privine), oxymetazoline (Afrin and others), phenylephrine (Coricidin and many others), tetrahydrozoline (Tyzine), and xylometazoline (Otrivin). Many of these are available as over-the-counter (OTC) preparations. The choice of a topical nasal decongestant varies among people. Some patients may have no response to one and respond well to another.
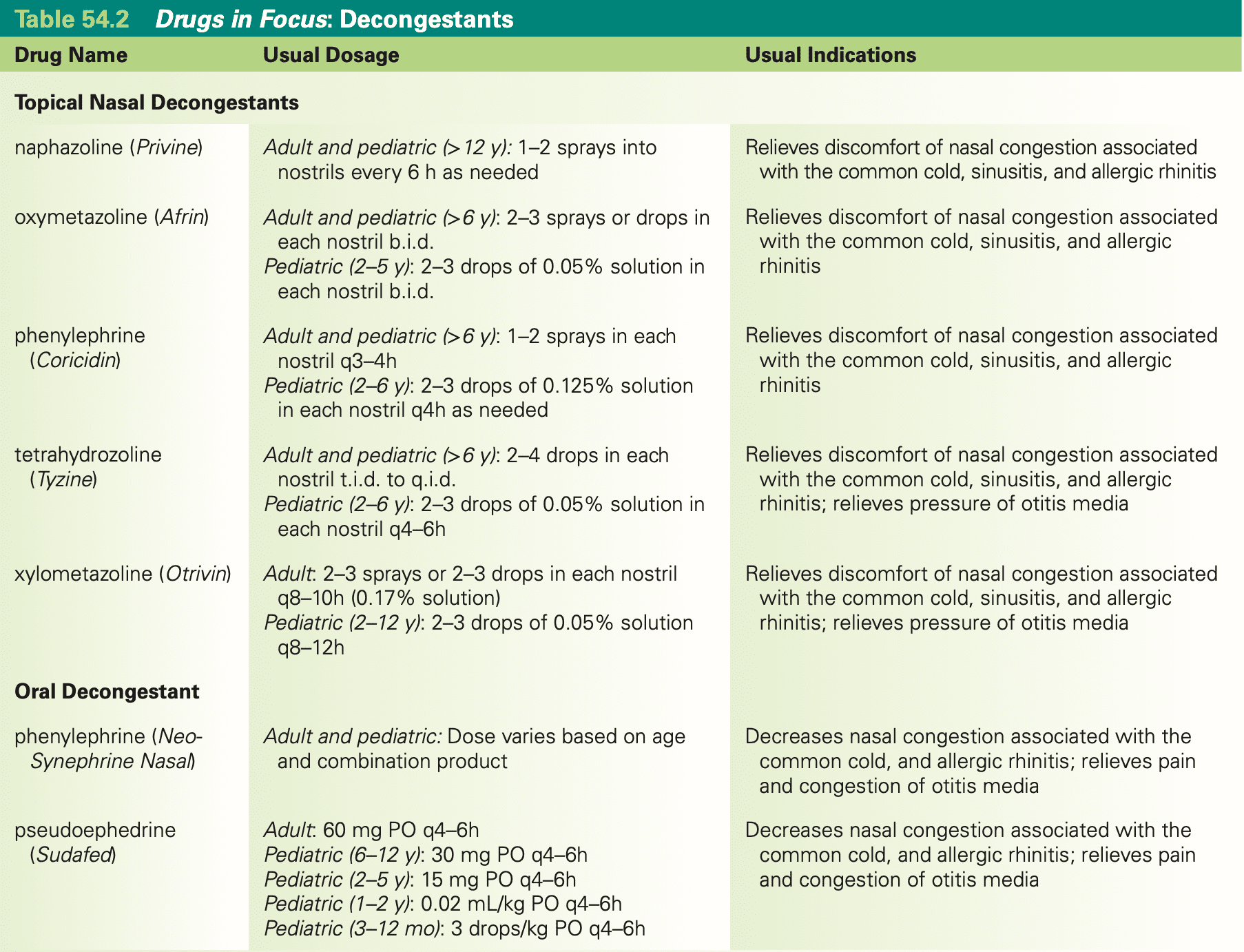
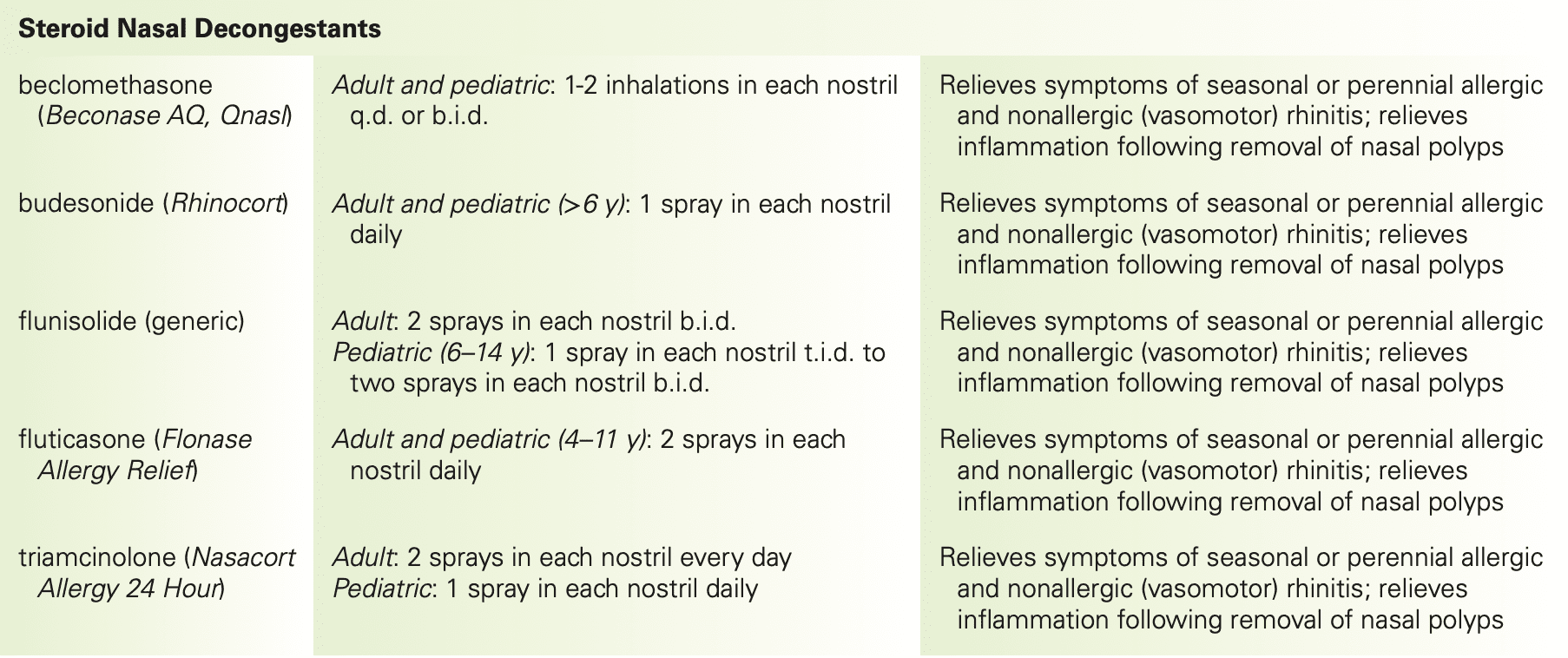
Topical decongestants are sympathomimetics, meaning they imitate the effects of the sympathetic nervous system to cause vasoconstriction, leading to decreased edema and inflammation of the nasal membranes. They are available as nasal sprays that are used to relieve the discomfort of nasal congestion that accompanies the common cold, sinusitis, and allergic rhinitis. These drugs can also be used when dilation of the nares is desired to facilitate medical examination or to relieve the pain and congestion of otitis media. Opening the nasal passage allows better drainage of the eustachian tube, relieving pressure in the middle ear. See Table 54.2 for usual indications for each of these agents.
Box 54.2 Focus on Patient and Family Teaching
ADMINISTERING NASAL MEDICATIONS
Proper administration technique is important for assuring that drugs given nasally have the desired therapeutic effect. It is important to periodically check the nares for any signs of erosion or lesions, which could allow systemic absorption of the drug. Most patients prefer to self-administer nasal drugs, so patient teaching is important. Explain the technique, and then observe the patient using the technique.
Because these drugs are applied topically, the onset of action is almost immediate and there is less chance of systemic effects. Although they are not generally absorbed systemically, any portion of these topical decongestants that is absorbed is metabolized in the liver and excreted in the urine. See Box 54.2 for tips on how to teach patients to use these medications.
Caution should be used when there is any lesion or erosion in the mucous membranes that could lead to systemic absorption. Caution should also be used in patients with any condition that might be exacerbated by sympathetic activity, such as glaucoma, hypertension, diabetes, thyroid disease, coronary disease, or prostate problems, because these agents have adrenergic properties. Because there are no studies regarding the effects of these topical drugs in pregnancy or lactation, if used during pregnancy or lactation, caution is advised.
Adverse effects associated with topical decongestants include local stinging and burning, which may occur the first few times the drug is used. If the sensation does not pass, use should be discontinued because it may indicate lesions or erosion of the mucous membranes. Use for longer than 3 to 5 days can lead to a rebound congestion (also called rhinitis medicamentosa), which occurs when the nasal passages become congested as the drug effect wears off. As a result, patients tend to use more drug to decrease the congestion, thus initiating a cycle of congestion–drug–congestion, which leads to abuse of the decongestant. Sympathomimetic effects (e.g., increased pulse and blood pressure; urinary retention) should be monitored because some systemic absorption may occur, though these effects are less likely with topical administration than with other routes.
The use of topical nasal decongestants with other medications that affect the sympathetic nervous system should be monitored carefully.
Nursing conclusions related to drug therapy might include
Question
What should be monitored to evaluate for urinary retention in patients receiving drug therapy?
Answer the question above the continue reading. iTELL evaluation is based on AI and may not always be accurate.
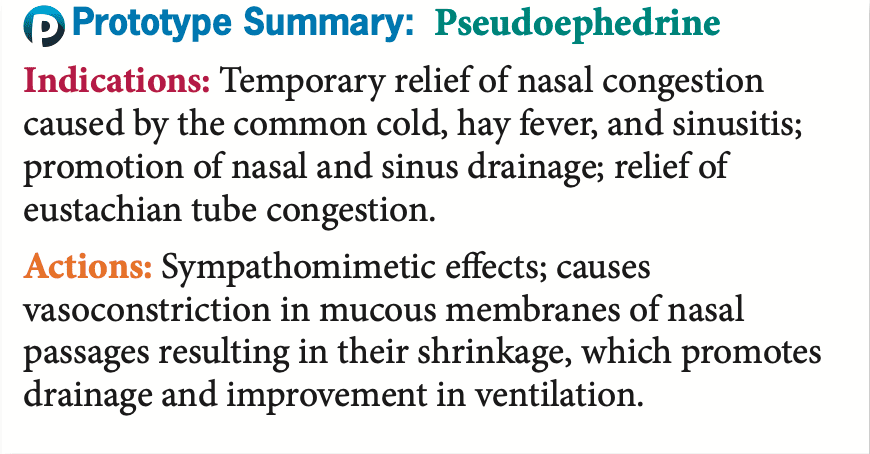
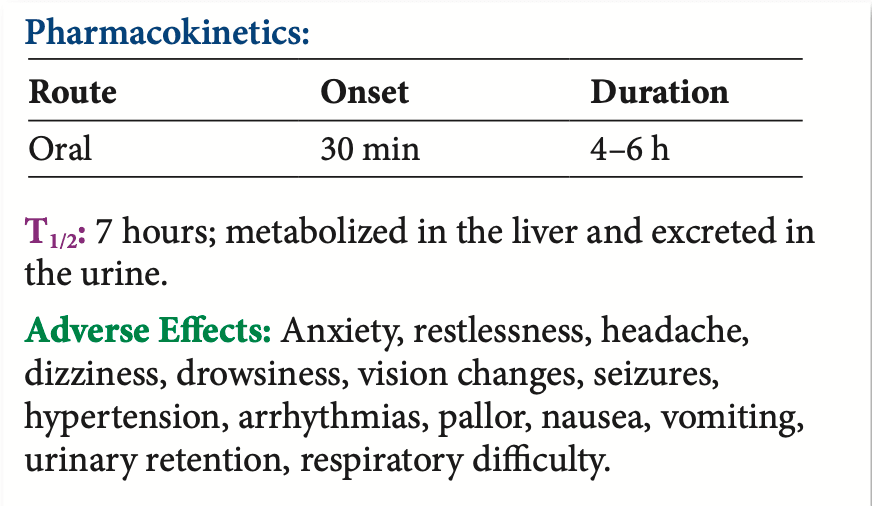
The oral decongestants currently available for use are pseudoephedrine and phenylephrine (Sudafed and many combination products) (see Table 54.2).
Oral decongestants are drugs that are taken orally to decrease nasal congestion related to the common cold, sinusitis, and allergic rhinitis. They are also used to relieve the pain and congestion of otitis media. Opening of the nasal passage allows better drainage of the eustachian tube, relieving pressure in the middle ear.
Oral decongestants shrink the nasal mucous membrane by stimulating the alpha-adrenergic receptors in the nasal mucous membranes. This shrinkage results in a decrease in membrane size, promoting drainage of the sinuses and improving airflow.
Pseudoephedrine is generally well absorbed and reaches its peak level quickly, in 20 to 45 minutes. It is widely distributed in the body, metabolized in the liver, and primarily excreted in the urine. Phenylephrine is available in a nasal spray and combination products.
Because these medications have adrenergic properties, caution should be used in patients with any condition that might be exacerbated by sympathetic activity, such as glaucoma, hypertension, diabetes, thyroid disease, coronary disease, and prostate problems. Because there are no adequate studies about use during pregnancy and lactation, such use should be reserved for situations in which the benefit to the patient outweighs any potential risk to the fetus or neonate.
Adverse effects associated with these decongestants include rebound congestion. Because these drugs may be taken systemically, adverse effects related to the sympathomimetic effects are more likely to occur, including feelings of anxiety, tenseness, restlessness, tremors, hypertension, arrhythmias, sweating, and pallor. Pseudoephedrine is found in many “behind-the-counter” cold and fl u preparations, and phenylephrine is OTC, so care must be taken to avoid inadvertent overdose when more than one such drug is used. Th ere are safety measures in place limiting access to pseudoephedrine (Box 54.3).
Box 54.3 Focus on Safe Medication Administration
The ingredient pseudoephedrine has been used to make methamphetamine, so there are federal and state laws restricting sales amounts. Medications with pseudoephedrine are designated “behind-the-counter” instead of OTC. To procure a behind-the-counter medication, a patient does not need a prescription. However, the medications are sold in limited quantities and a pharmacist must allow access. This policy helps to limit the amount of pseudoephedrine that a person can buy. There are many cough and allergy OTC products that contain a combination of medications, so patients need to be able to read labels to be cautious when treating these symptoms without assistance from a provider and/or pharmacist.
Many behind-the-counter and OTC products, including cold remedies, allergy medications, and fl u remedies, may contain pseudoephedrine or phenylephrine. Taking such products concurrently can cause serious adverse effects. Teach patients to read the labels to avoid inadvertent overdose.
Nursing conclusions related to drug therapy might include
Topical nasal steroid decongestants (see Table 54.2 ) include beclomethasone (Beconase AQ and others), budesonide (Rhinocort), flunisolide (generic), fluticasone (Flonase Allergy Relief), and triamcinolone (Nasacort Allergy 24 Hour).
Topical nasal steroid decongestants are used for the treatment of allergic rhinitis and to relieve inflammation after the removal of nasal polyps. They are first-line medications for nasal congestion. The exact mechanism of action of topical steroids is not known. Their anti-inflammatory action results from their ability to produce a direct local effect that blocks many of the complex reactions responsible for the infl ammatory response.
The onset of action is not immediate, and these drugs may actually require up to 1 week to cause any changes. If no effects are seen aft er 3 weeks, the drug should be discontinued. Because these drugs are not generally absorbed systemically, their pharmacokinetics are not reported. If they were to be absorbed systemically, they would have the same pharmacokinetics as other steroids (see Chapter 36).
Because nasal steroids block the inflammatory response, their use is contraindicated in the presence of acute infections. Increased incidence of Candida albicans infection has been reported with their use related to the anti-inflammatory and anti-immune activities associated with steroids. Caution should be used in any patient who has an active infection, including tuberculosis, because systemic absorption would interfere with the inflammatory and immune responses. Patients using nasal steroids should avoid exposure to any airborne infection, such as chickenpox or measles. As with all drugs, caution should always be used when taking these drugs during pregnancy or lactation, but because the systemic absorption of these drugs is minimal, they are oft en used during pregnancy and lactation.
Because they are applied topically, there is less chance of systemic absorption and associated adverse effects. The most common adverse effects are local burning, irritation, stinging, dryness of the mucosa, and headache. Because healing is suppressed by steroids, patients who have recently experienced nasal surgery or trauma should be monitored closely until healing has occurred.
The steroid nasal decongestants are applied topically and thus do not typically interact with other systemic medications. However, concurrent nasal medications should not be administered without discussion with a health care provider.


Question
What are the therapeutic actions and indications for topical nasal steroid decongestants?
Answer the question above the continue reading. iTELL evaluation is based on AI and may not always be accurate.
Nursing conclusions related to drug therapy might include
● Decongestants cause local vasoconstriction, thereby reducing blood fl ow to the mucous membranes of the nasal passages and sinus cavities.
● Rebound vasodilation (rhinitis medicamentosa) is an adverse effect of excessive or long-term decongestant use.
● Topical nasal decongestants are preferred for patients who need to avoid the systemic adrenergic effects associated with oral decongestants.
● Topical nasal steroid decongestants block the inflammatory response and are preferred for patients with allergic rhinitis.
Antihistamines (Table 54.3) block the release or action of histamine, a chemical released during inflammation that increases secretions and narrows airways. Antihistamines are found in multiple OTC preparations that are designed to relieve respiratory symptoms and to treat symptoms of allergies. When choosing an antihistamine, the individual patient’s reaction to the drug is usually the governing factor. Because first-generation antihistamines have greater anticholinergic effects with resultant drowsiness, a person who needs to be alert should be given one of the second-generation, less-sedating antihistamines. In some people, the second-generation antihistamines are also sedating, so care must be taken until the patient knows what response will occur. Because of their OTC availability, these drugs are often misused to treat colds and influenza (Box 54.4).
First-generation antihistamines include brompheniramine (J-Tan and others), carbinoxamine (Karbinal ER), chlorpheniramine (Aller-Chlor and others), clemastine (Dayhist Allergy), cyproheptadine (generic), dexchlorpheniramine (generic), dimenhydrinate (Dimentabs and others), diphenhydramine (Benadryl and others), hydroxyzine (Vistaril and others), meclizine (Antivert), promethazine (Phenergan), and triprolidine (generic).
Second-generation antihistamines include azelastine (Astelin, Astepro), cetirizine (Zyrtec), desloratadine (Clarinex), fexofenadine (Allegra), levocetirizine (Xyzal), loratadine (Claritin), and olopatadine (Patanase).


Antihistamines selectively block the effects of histamine at the histamine-1 receptor sites, decreasing the allergic response. They also have anticholinergic and antipruritic effects. Antihistamines are used for the relief of symptoms associated with seasonal and perennial allergic rhinitis, allergic conjunctivitis, uncomplicated urticaria, and angioedema. They are also used for the amelioration of allergic reactions to blood or blood products, for relief of discomfort associated with dermographism, and as adjunctive therapy in anaphylactic reactions. They are most effective for symptoms of itching, sneezing, and rhinorrhea. Some can be used to treat or prevent motion sickness and insomnia. See Table 54.3 for usual indications for each of these agents. Other uses that are being explored include relief of exercise- and hyperventilation-induced asthma and histamine-induced bronchoconstriction in asthmatics. They are most effective if used before the onset of symptoms.
Box 54.4 Focus on Patient and Family Teaching
Following reports of serious and even fatal adverse effects when OTC cough and cold medicines were used in children under the age of 2 years, the FDA held meetings to evaluate the safety and efficacy of the use of these products in young children. The evidence continues to be evaluated, and current recommendations include the following:
Antihistamines are well absorbed orally with an onset of action ranging from 1 to 3 hours. Th ey are generally metabolized in the liver, with excretion in the feces and urine. These drugs cross the placenta and enter human milk (see “Contraindications and Cautions”).
Antihistamines are contraindicated during pregnancy or lactation unless the benefit to the patient clearly outweighs the potential risk to the fetus or baby. Some of the medications have higher safety profiles than others, so medication labels should be evaluated to determine risk of use during pregnancy and/or lactation. Some should be used with caution, and there may need to be dosage adjustment for patients with renal or hepatic impairment, which could alter the metabolism and excretion of the drug. Special care should be taken when some of the first-generation antihistamines are used by a patient with a history of arrhythmias or prolonged QT intervals because fatal cardiac arrhythmias have been associated with the use of certain antihistamines and drugs that increase QT intervals, including erythromycin. Box 54.4 presents topics for patient education in the use of these OTC products.
The adverse effects most often seen with antihistamine use are drowsiness and sedation (see “Critical Thinking Scenario” for additional information), though second-generation antihistamines are less sedating in many people. The anticholinergic effects that can be anticipated include drying of the respiratory and GI mucous membranes, GI upset and nausea, arrhythmias, dysuria, urinary hesitancy, and skin eruption and itching associated with dryness.
Drug–drug interactions vary among the antihistamines; for example, anticholinergic effects may be prolonged if diphenhydramine is taken with an MAO inhibitor, and the interaction of fexofenadine with ketoconazole or erythromycin may raise fexofenadine concentrations to toxic levels. Concurrent use with other CNS depressants can increase the sedative effect of the antihistamines. For more information, consult a nursing drug handbook or package insert for individual details.


K.E. is a 46-year-old patient who has been self-treating for seasonal rhinitis and a cold. Their spouse calls the physician’s offi ce, concerned that K.E. is dizzy, has lost their balance several times, and is very drowsy. K.E. is unable to drive to work or to stay awake. K.E.’s spouse wants to take K.E. to the emergency department of the local hospital.
The first impression of K.E.’s condition is that it is a neurological disorder. K.E. should be evaluated by a health care provider to rule out signifi cant neurological problems. However, after a careful patient history and physical examination, K.E.’s condition seemed to be related to high levels of OTC medications.
There are a multitude of OTC cold and allergy remedies, most of which contain the same ingredients in varying proportions. A patient may be taking one to stop their nasal drip, another to help their cough, another to relieve congestion, and so on. By combining OTC medications like this, a patient is at great risk for inadvertently overdosing or at least allowing the medication to reach toxic levels.
In this situation, the fi rst thing to determine is exactly what medications are being taken and how often. K.E. seems to have suffered from adverse reactions to the antihistamines, decongestants, or other upper respiratory tract agents. The nurse should encourage K.E.—and all patients—to check the labels of any OTC medications being taken and to check with the health care provider if there are any questions. K.E. and their spouse should receive written information about the drugs that K.E. is taking. They also should be shown how to read OTC bottles or boxes for information on the contents of various preparations. In addition, they should be encouraged to use alternative methods to relieve the discomfort of seasonal rhinitis (e.g., using a humidifier, drinking lots of liquids, and avoiding smoky areas) to allay the belief that many OTC drugs are needed. Finally, K.E. and their spouse should be advised to check with their health care provider if they have any questions about OTC or prescription drugs or if they have continued problems coping with seasonal allergic reactions. Other prescription medication may prove more effective.
Assess K.E.’s health history for allergies and GI stenosis or obstruction, bladder obstruction, narrow-angle glaucoma, benign prostatic hypertrophy, and concurrent use of MAO inhibitors and OTC allergy or cold products.
Focus the physical examination on
CNS: Orientation, refl exes, affect, coordination
Skin: Lesions
CV: Blood pressure, pulse, peripheral perfusion
GI: Bowel sounds, abdominal exam
Hematological: Complete blood count
Respiratory: Respiratory rate and character, nares, adventitious sounds
Genitourinary (GU): Urinary output
Impaired comfort related to GI effects or dry mouth
Altered sensory perception (kinesthetic)
Safety risk due to dizziness and/or sedation
Knowledge defi cit regarding drug therapy
The patient will receive the best therapeutic effect from the drug therapy.
The patient will have limited adverse effects from the drug therapy.
The patient will have an understanding of the drug therapy, adverse effects to anticipate, and measures to relieve discomfort and improve safety.
Provide comfort and safety measures (e.g., reduce risk of falls and GI discomfort); teach about mouth care; increase humidity.
Provide support and reassurance to deal with drug effects and allergy.
Provide patient teaching regarding drug name, dosage, adverse effects, precautions, and warning signs to report.
Evaluate drug effects (relief of respiratory symptoms).
Monitor for adverse effects: CNS effects, thickening of secretions, urinary retention, constipation, sedation, dizziness, glaucoma.
Monitor for drug–drug interactions as indicated.
Evaluate the effectiveness of support and encouragement strategies, patient teaching program, and comfort and safety measures.
Question
What could be causing the drowsiness and dizziness in K.E.?
Answer the question above the continue reading. iTELL evaluation is based on AI and may not always be accurate.
● Antihistamines selectively block the effects of histamine at the histamine-1 receptor sites, decreasing the allergic response. Antihistamines are used for the relief of symptoms associated with seasonal and perennial allergic rhinitis, allergic conjunctivitis, uncomplicated urticaria, and angioedema.
● Patients taking antihistamines may have dryness of the skin and mucous membranes. The nurse should encourage them to drink plenty of fluids, use a humidifier if possible, avoid smoke-filled rooms, and use good skin care and moisturizers.
● Some first-generation antihistamines should be avoided with any patient who has a prolonged QT interval because serious cardiac complications and even death have occurred.
Expectorants (Table 54.4) increase productive cough to clear the airways. They liquefy lower respiratory tract secretions, reducing the viscosity of these secretions and making it easier for the patient to cough them up. Expectorants are available in many OTC combination preparations, making them widely available to the patient without advice from a health care provider. Currently, the only available expectorant sold outside of the combination formulations is guaifenesin (Mucinex).

Guaifenesin enhances the output of respiratory tract fluids by reducing the adhesiveness and surface tension of these fluids, allowing easier movement of the less viscous secretions. The results of this thinning of secretions are a more productive cough and enhanced patency of the respiratory airways. See Table 54.4 for usual indications.
Guaifenesin is rapidly absorbed with an onset of 30 minutes and a duration of 4 to 6 hours. Sites of metabolism and excretion have not been reported.
This drug should not be used in patients with a known allergy to the drug to prevent hypersensitivity reactions, and it should be used with caution in pregnancy and lactation because of the potential for adverse effects on the fetus or baby and with persistent coughs, which could be indicative of underlying medical problems.
The most common adverse effects associated with expectorants are GI symptoms (e.g., nausea, vomiting, anorexia). Some patients experience headache, dizziness, or both. A rash may be a sign of an allergic reaction. The most important consideration in the use of these drugs is diagnosing the cause of the underlying cough. Prolonged use of OTC preparations could result in the masking of important symptoms of a serious underlying disorder. These drugs should not be used for more than 1 week; if the cough persists, encourage the patient to seek health care.
There are no known significant drug interactions with guaifenesin. However, patients should be cautioned that there may be drug interactions with other medications that guaifenesin is combined with in OTC formulations.

Nursing conclusions related to drug therapy might include
● Expectorants are drugs that liquefy respiratory tract secretions. They are used for the symptomatic relief of respiratory conditions in which thick mucus exacerbates cough and decreases airway patency.
● Guaifenesin is the only expectorant currently available. Care should be taken to avoid inadvertent overdose when using OTC and/or combination products that contain this drug.
Mucolytics (Table 54.5) increase or liquefy respiratory secretions to aid the clearing of the airways in high-risk respiratory patients who are coughing up thick, tenacious secretions. Patients may be suffering from conditions such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, pneumonia, or tuberculosis. Mucolytics include acetylcysteine (generic) and dornase alfa (Pulmozyme).

Acetylcysteine is used orally or intravenously to protect liver cells from being damaged during episodes of acetaminophen toxicity because it normalizes hepatic glutathione levels and binds with a reactive hepatotoxic metabolite of acetaminophen. Acetylcysteine affects the mucoproteins in the respiratory secretions by splitting apart disulfidebonds that are responsible for holding the mucus material together. The result is a decrease in the tenacity and viscosity of the secretions. See Table 54.5 for usual indications.
Dornase alfa is a mucolytic prepared by recombinant DNA techniques that selectively break down respiratory tract mucus by separating extracellular DNA from proteins. It is used in cystic fibrosis, which is characterized by thick, tenacious mucous production. See Table 54.5 for usual indications. See Box 54.5 for information about targeted treatment of cystic fibrosis.
The medication may be administered by nebulization or by direct instillation into the trachea via an endotracheal tube or tracheostomy.
Acetylcysteine is metabolized in the liver and excreted somewhat in the urine. It is not known whether it crosses the placenta or enters human milk. Dornase alfa is metabolized by proteases, and its half-life is 3 to 4 hours.
Box 54.5 Targeted Treatment of Cystic Fibrosis
Between 2012 and 2019, several medications were approved by the FDA for treatment of cystic fi brosis. Ivacaftor (Kalydeco) and combination medications that include ivacaftor (Orkambi, Symdeko, and Trikafta) are designed as targeted treatment for patients with cystic fibrosis. Ivacaftor is a cystic fibrosis transmembrane conductance regulator (CFTR) that facilitates increased chloride transport at the surface of epithelial cells in multiple organs. In cystic fibrosis patients taking this drug, the end result was improved lung function. Ivacaftor is approved for patients 4 months of age and older who have a type of CFTR gene mutation that is responsive to ivacaftor. If the patient’s genotype is not known, tests should be run to attempt to detect a CFTR mutation. The FDA has approved a cystic fi brosis mutation test that can be used to determine the appropriateness of this drug. It is an oral agent and needs to be used with caution in patients with liver impairment or those also using CYP3A inhibitors. The most common adverse effects include abdominal pain, rash, nausea, dizziness, headache, and sore throat. A serious but rare effect can be the development of non-congenital lens opacities/cataracts in pediatric patients.
The medications are contraindicated in patients who have history of hypersensitivity reactions to the medications or components in the medications. Caution should be used with patients who have asthma due to potential for bronchospasm. There are no adequate human studies to evaluate risk during pregnancy or lactation, but there has been no evidence of fetal harm in animal studies.
Adverse effects most commonly associated with mucolytic drugs include GI upset, stomatitis, rhinorrhea, bronchospasm, and occasionally a rash.
There are no known drug interactions with acetylcysteine or dornase alfa.

Nursing conclusions related to drug therapy might include
● Mucolytics work to break down mucus to aid high-risk respiratory patients in coughing up thick, tenacious secretions.
● Dornase alfa is specific for the treatment of patients with cystic fibrosis, which is characterized by a thick, tenacious mucus production that can block airways.
Question
What should nurses evaluate when assessing a patient's history and physical examination related to drug therapy?
Answer the question above the continue reading. iTELL evaluation is based on AI and may not always be accurate.
Last updated at